Men and their experiences living with hypermobile Ehlers Danlos syndrome is a whole topic…one that doesn’t get nearly enough attention in my opinion. When you look online for info about guys and hEDS, for instance, there just isn’t a lot of useful material. Nobody is denying that guys can have EDS, but the disorder is associated more readily with women and there is a pervasive notion that male persons don’t suffer as much as female ones when living with disordered collagen.
As a practitioner of Chinese medicine with over a decade of experience working with EDS and hypermobile (HSD) patients, I do not agree with received wisdom about men and hEDS.1 I don’t think it’s as rare as it’s posited to be, for one thing. I do see in my guy patients and clients some factors that pertain directly to sex and gender. I don’t see it as a competition. With EDS, there is enough disruption and dysfunction for everyone involved, no need to squabble over it.
(Just out of curiosity…If you are a guy with EDS, what differences do you see between your experiences and those of female persons? And of these differences, which ones matter the most to you?)
Prevalence
If I only consider my diagnosed patients and health coaching clients, then yes, I work more with women than with men. But if I count undiagnosed patients and clients who show clear evidence of EDS/HSD, the percentage shifts. It really is not all that uncommon for guys to be hypermobile, if not clearly presenting within the rubric that delineates hEDS/HSD.
I have noticed that the diagnosed guys tend to feel isolated in their experience with EDS. They don’t necessarily have a community of other guys just like them. The undiagnosed guys show a range of presentations and approaches to their own wellbeing. Some are aware of hEDS/HSD and recognize that they may very well be living with it. Others are oblivious to the disorder and only recognize that they are in pain or are otherwise struggling… no idea why. Either way, they don’t have it as easy as a guy who comes to see me for normie concerns. Being hypermobile, especially when the usual comorbid conditions are also present, has some unique nuances when we consider men and their experiences as a result of it.
That doesn’t mean it’s all tragedy or doom and gloom. It is different, that’s all.
“And when he turned 17, Daniel ran away to join the circus to kickstart his career as a contortionist – going on to train under Master Lu Yi at the San Francisco School of Circus Arts. ‘I joined a circus when I was 17, and I’ve travelled the entire world,” the contortionist smiled. “It’s just been absolutely phenomenal.’”
Daniel Browning Smith, performance artist
How Does It Present?
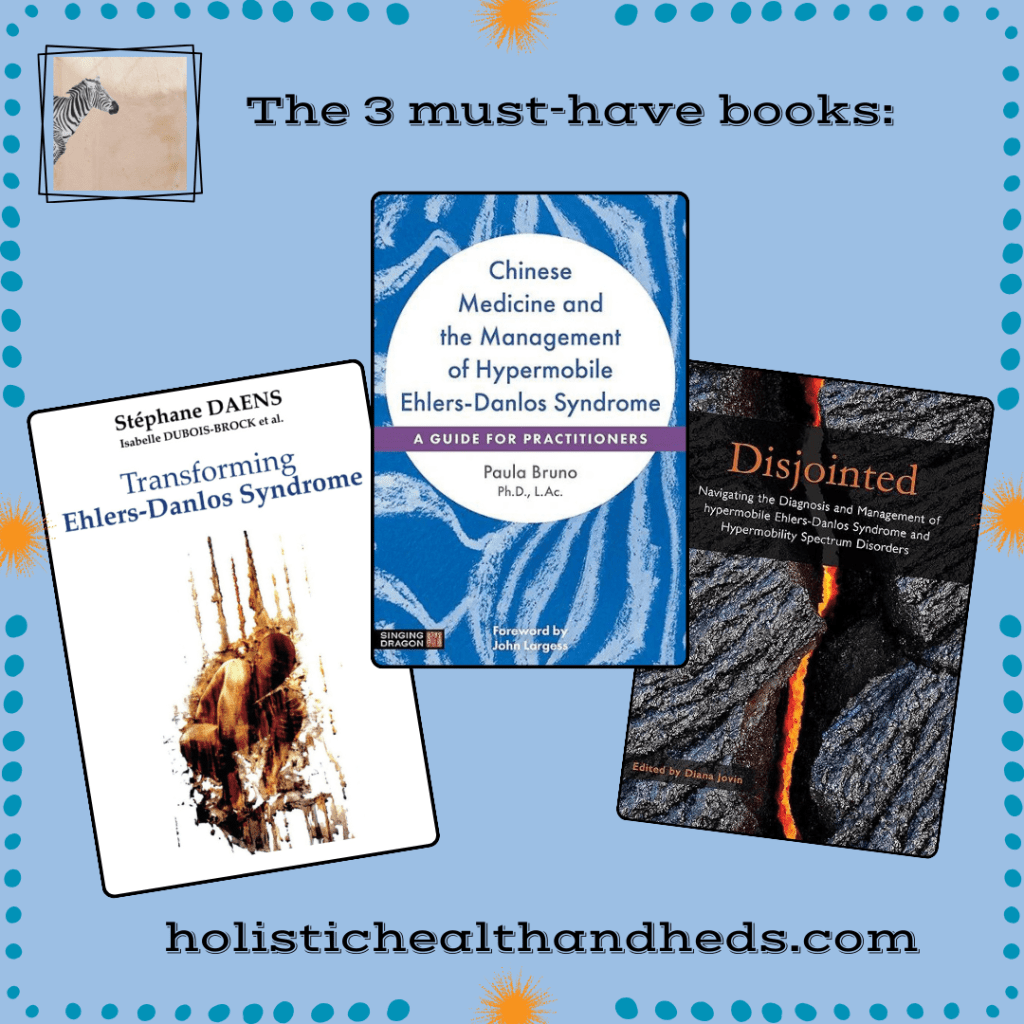
I do get male patients or clients (those would be folks who work with my in my capacity as a health coach) who find me either via my book, Chinese Medicine and the Management of Hypermobile Ehlers Danlos Syndrome, or through either this website or my original one, Two Hearts Wellness. We begin at the beginning: they have hEDS and want support to improve their health. It is a matter of a diagnosed condition and how it is affecting them, and that’s that. Others are not diagnosed but, over time, a pattern of symptoms and signs present that make diagnosis if not inevitable then at least possible.
Diagnosed or not, how being a guy with hEDS/HSD can manifest in three key areas–namely, pain, the pelvic floor, and gut health–is the focus of this particular blog post. It won’t be the only time I write about guys and EDS, though. This is a topic that merits attention and respect and I will for sure return to it in future essays.
“Unlike some of his competitors, Gilliver uses a wheelchair due to Ehlers-Danlos Syndrome, a rare condition affecting connective tissue.”
Piers Gilliver, British Paralympic fencer
Pain & Gender Performance:
Keep in mind that I specialize in men’s health anyway, so guys come to me because they are in pain. This can be a matter of chronic illness-related pain or it can be the kind anyone suffers after an injury or illness or any other normie root cause.
Men have different ways of articulating their pain. Acceptable pain is when a guy breaks his leg playing football. Less-acceptable pain is having loose joints and unending low-grade inflammation that leaves a guy tired and suffering for months on end. It’s ok and still manly if there is a clear cause and effect (and resolution) to pain, and behaving like a dramatic five-year-old when one has a cold or the flu is an acceptable, albeit clichéd, response. Chronic pain, on the other hand, tends to be minimized.
“‘As I struggled with incurring and recovering from various joints injuries over the last several year, I thought I was just unlucky,’ he said.
—Chaz Lucius, athlete
‘With this diagnosis of EDS, I now realize that my body impacted by EDS could not handle the physical nature of playing hockey. Given this condition, my injury history, and the physical nature of hockey, I have been medically advised not to continue to play.’”
Or at least…that’s the way some guys see it. Gender norms for experiencing pain and expressing it definitely do affect how a guy filters his experiences with EDS/HSD. This does color how guys experience healthcare systems and their own wellbeing (or lack) too. I’ve had patients who had repeated shoulder subluxations to the extent that it was almost like the arm was going to fall off, for example, and the male patients were the ones who completely and totally–and to me, shockingly–minimized their experience.2
There’s a difference between minimizing pain because we’re used to it (don’t we all do that when we live with hEDS/HSD and chronic pain?) and brushing off pain because you’ve internalized messages like “boys don’t cry” and “shake it off, it’s not like you’re dying here.” Part of creating ways to live better and more comfortably, at least in my practice, consists of helping guys to be present for their pain in a healthy way.
What’s Up With The Undercarriage?
In terms of reproductive and sexual health, guys with hEDS/HSD may struggle with erectile dysfunction (ED), pelvic floor problems of all kinds, infertility, and/or low libido. This list of issues is not so different from anything I’d treat in the normie population, but hEDS/HSD–once again–gives a special tone to any of these concerns. Is it a hormone problem…or is it dysautonomia? Maybe the person has pelvic floor dysfunction because their posture is terrible or as a result of an injury. With hEDS/HSD, the problem might instead be caused by weak ligaments due to collagen dysfunction. And so forth.
For better or for worse, women are more accustomed to getting our undercarriages examined. It’s also easier to find a pelvic floor therapist when one is female. For guys, even being aware of their pelvic floor might take some doing, much less paying mindful attention to it in a wellbeing practice.
“This is not an old person’s disease. I want to make sure everyone understands that because there are people in their 20s that have developed the symptoms that I have in my 50s.”
Drake Jensen, country music artist
All persons, whether or not they have male genitalia and identify as male, can benefit from greater awareness of their pelvic floor. Guys with any version of EDS have extra cause to learn about this region. From wanting to be stable and centered (form and function) to reproductive and sexual health to having the ability to urinate and/or have a healthy bowel movement, the pelvic floor is not an area that someone with EDS can safely ignore.3
Gut Health (Or Not):
Guys with hEDS/HSD do not tend to have it any easier or any harder than do female persons or anyone else in between when it comes to middle section misery.4 If you have problems, you have problems. Is MCAS an issue? What about dysautonomia? Gastroparesis is the same. If you live with any of these conditions, they are no fun. Of course, women are more frequently diagnosed with the above-mentioned, but if it’s a question of living with these issues or not? If you live with them, you know: they can make your life really, really challenging.
Gut health is one of my favorite subjects, actually, and I have a special affinity for MCAS sufferers. I am one and I’ve had a long and challenging road while figuring out how to ameliorate its effects on my life.5 As with pain and the undercarriage, gut health in a person with EDS requires parsing out the individual’s own version of stable health–(what is normal for that person?)–and then strategizing and building upon what strengths that person does have. And there are always strengths and footholds. It just takes some time to find them and experiment with options that work for that unique person.
*****
*****
What my clinical experience has shown me–over and over–is that guys tend not to want to give things a name. They are not as inclined to embrace the terminology or a diagnosis, per se. But they do know (how can a person not know?) when they have MCAS-related diarrhea or incredibly slow digestion or intractable constipation. Men also seem a little slower to embrace the notion of gut health being whole-self health but (at least in my experience) there seems to be a lesser risk of becoming orthorexic in my male patients and clients, and they also seem a bit less scarred by being gaslit by their MD over weight than are women.
No matter the sex or gender, though, gut health and how to achieve it is a primary concern in any treatment strategy that I create for patients or clients with hEDS/HSD.
In Conclusion (For Now)
Everyone who lives with EDS, MCAS, and/or POTS has a hard row to hoe. Maybe you’re diagnosed, maybe you have a long history of being gaslit as you try to get diagnosed. It could be that you were a normie until you got a whiplash injury or a concussion.6 There are a lot of roads that lead not to Rome, but–instead–to chronic illness. And here you are.
“Injured times and well times (or at least less-injured times) generally juxtapose in a back-and-forth flow, something rather different from the more conventional paradigm of expecting perpetual robust health to be a default state […]”
Noah Baerman, jazz pianist & composer
Yes, biological sex is a factor and where you are on the spectrum of it does make a difference. Gender does the same. From feeling isolated to finding a community (if that is what you want), to not being able to access treatment that works for your vision of yourself, to creating your own wellness strategy with someone who understands you and has experience with men’s health, yes…sex and/or gender is a puzzle piece that may be a significant one for you.
Received wisdom holds that men have any easier time with hEDS/HSD and that they experience this condition less than women do. My response? Meh. If you’re a guy with hEDS/HSD or any of the routine comorbidities, then do you honestly care about the gendered aspects of living with hEDS/HSD as a man…or do you care about living your best life and becoming as healthy and well as is possible for you, a unique individual with experiences and needs of your own?
*****
*****

Dr. Paula Bruno, Ph.D., L.Ac., is a licensed acupuncturist and herbalist, an AOBTA-CP traditional Chinese bodywork therapist, an author, and a health coach. She maintains an active and growing practice at Two Hearts Wellness, her Austin, TX office. Dr. Bruno is also available for distance appointments for wellness consultation or coaching.
In her first career, she was a Spanish professor.
Dr. Bruno’s specialties as a Chinese medicine practitioner include: • Musculoskeletal health (acute or chronic pain relief; Ehlers Danlos syndrome & hypermobility support) • Digestive support, gut health, and weight loss • Aesthetic treatment, including scar revision • Men’s health • General preventative care and wellness support for all persons.
She is the author of Chinese Medicine and the Management of Hypermobile Ehlers Danlos Syndrome: A Practitioner’s Guide.
When you are ready to discover what traditional medicine plus a vibrant and engaged approach to holistic health can do for you, either contact Dr. Bruno or book an appointment online.
*****
*****
Two Hearts Wellness/Holistic Health & hEDS does not accept paid advertising on this website
Note: Material on this web site site is not intended to diagnose, prevent, treat, or cure any disease, illness, or ailment. A Chinese medicine practitioner in Texas identifies syndrome patterns but does not diagnose illness. Material on this web site does not purport to identify syndrome patterns.
*****
- This particular blog post focuses on cisgender men and hypermobile EDS but I feel it important to clarify that there are a number of topics pertaining to sex, gender, and EDS (and not just hEDS) that are significant but which do not fit into this particular essay. ↩︎
- The matter of sex, gender, and pain is a rabbit hole and too much for this essay. However, some of the issues at hand include the question of how men experience pain, and recent studies in chronic pain consider the mechanisms of this process, as we see in the 2024 study, “Self-regulated analgesia in males but not females is mediated by endogenous opioids.” Refer also to “Biological Mechanisms Underlying Sex Differences in Pain” (2024). A potentially relevant factor is that men are able to build muscle perhaps more readily that women (not always the case, but…), and muscle gives a layer of stability to and EDS body that a person without muscle tone would then lack. Another piece in the puzzle is the way that men are allowed (or not) to express pain and ask for help. Though women’s pain is more readily ignored and discounted in the medical setting, men have their own roadblocks to asking for and receiving meaningful support, as noted in “Men In Pain: How Ideals of Masculinity Harm Men With Chronic Pain.” ↩︎
- My interest in men’s health has deep roots, as outlined in “Men’s Health & Why It’s On My Radar (Thoughts From a Holistic Practitioner).” For excellent, thorough, and valuable information about men’s health and hEDS, do take the time to watch “The Effects of EDS and HSD in Males.” The description of the video is as follows: “Adam Sherman, a nurse that also lives with Ehlers-Danlos Syndrome, will attempt to synthesize research, standard knowledge, and common sense to explore how biological, anatomical, environmental, and psychosocial differences can create unique challenges for males built with the connective tissue of EDS and HSD; it is intended for patients and their caregivers, family, friends, and healthcare teams. Not meant to be all-encompassing, the material will still attempt to consider all stages of development, sexual/gender identities within the male sex/gender and how it may be relevant to intersex individuals.” As a resource, this video truly valuable and I highly recommend it! ↩︎
- Again, we see that women are more inclined to develop gastroparesis than are men (see “Gender-Related Differences in Gastroparesis“) and experience POTS differently as well (“Biological sex-dependent differences in postural orthostatic tachycardia syndrome“). My feeling on the matter, though? It does not really matter what your sex and/or gender (or gender expression) is when you have MCAS, POTS, or gastroparesis. I have male patients with MCAS, POTS, and various gut health issues related to either slow emptying and/or being a mastie, and sex/gender doesn’t really matter after a certain point. What matters is that the patient or client is uncomfortable, they may be truly disabled by their gut issues, and/or their POTS or other dysautonomia presentations are hindering their enjoyment of life. That more women have it than do men, or that hormones and gender may make things different, isn’t the main concern when hearing a patient or client’s story and figuring out ways to improve their wellbeing. ↩︎
- Stay tuned for further blog posts about MCAS and gut health. To date, I’ve posted “Holidays and MCAS: Surviving and Thriving From November To January” and “Intuitive Eating vs. Mindful Eating–Which Is Better For You? (Some Tips For Folks With EDS, MCAS, &/or POTS)” on this website. On the home website, Two Hearts Wellness, a useful piece on what Chinese medicine can do for gut health is “Gut & Digestive Health: Three Reasons Why It Matters & How Chinese Medicine Can Improve Yours.” ↩︎
- As many of us already know, there have been some intriguing findings on the genetic front but there is still no genetic test for hEDS. In addition, there are multiple possibilities as to the cause of this particular iteration of EDS. One is sustaining a concussion or whiplash. For discussion of the six most prevalent theories regarding hEDS, including the role of acute injury and epigenetics, see “What Causes Hypermobile Ehlers Danlos Syndrome? (A Summary of Theories).” ↩︎
